The Research Programme
Dr Keith Pine continues to investigate prosthetic eye wear as an honorary Research Fellow with the School of Optometry and Vision Science, University of Auckland. In the recent past he carried out a systematic investigation into the causes and management of mucoid discharge associated with prosthetic eye wear. This research involved 494 prosthetic eye wearers from throughout NZ and 335 clinical sessions. Dr Pine took 1340 photographs of sockets, companion eyes and stained prosthetic eyes during the course of this research and published 8 peer reviewed papers plus a book.
Of course , the research was aided enormously by Dr Pine’s supervisors and co-authors; Drs Robert Jacobs and Brian Sloan and the following organisations: The Multiregional Ethics Committee of the MOH, the University of Auckland Human Participants Ethics Committee, Auckland DHB, Capital & Coast DHB, Lakes DHB, Canterbury DHB, Waikato DHB, the NZ Accident Compensation Corporation and the Royal New Zealand Foundation of the Blind.
The research began with a survey of anophthalmic patients to confirm a research focus that most reflected their needs. The results of the survey highlighted the concerns that patients had at the time of eye loss as well as their on-going concerns after at least two years of prosthetic eye wear. Health of the remaining eye was their greatest concern at both occasions in time, but second on their list of on-going concerns was anxiety about mucoid discharge associated with their prosthesis. Frequent, viscous discharge affects the quality of life of prosthetic eye wearers as it can be difficult to live with a continuously suppurating eye that requires constant wiping.
View the article here: Concerns of anophthalmic patients wearing artificial eyes.

Stained tear protein deposits on a scleral shell prosthesis.
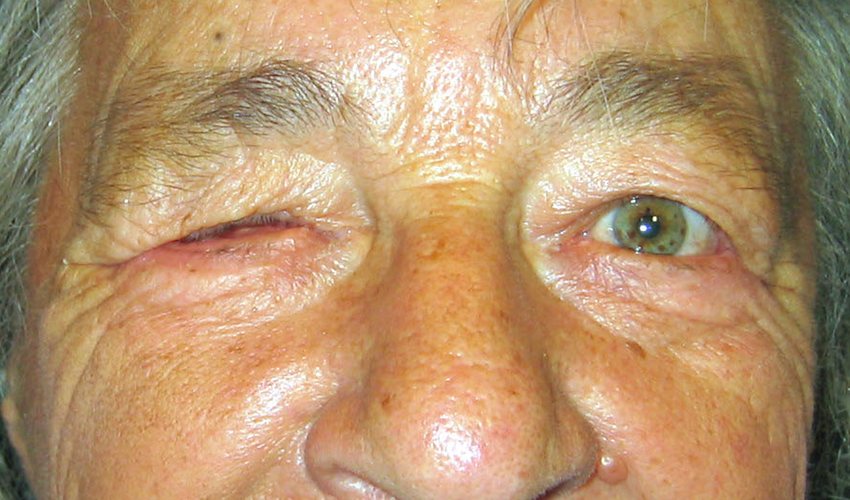
A small sample of the many patients who took part in the research
Because of the high level of concern about discharge expressed by patients, mucoid discharge associated with prosthetic eye wear was confirmed as a worthwhile research topic; however the scale of the problem amongst the anophthalmic population remained unknown. Also unknown were the demographics of anophthalmic patients, the aetiology of eye loss and eye loss trends in New Zealand. A second survey, larger than the first, was undertaken and 430 prosthetic eye wearers from throughout New Zealand completed a questionnaire about their experiences with ocular prostheses. Included with the questionnaire was an invitation to participate in further prosthetic eye research and 330 prosthetic eye wearers agreed to do so. The results of this survey confirmed that mucoid discharge associated with prosthetic eye wear was indeed high on patients’ list of concerns and that mucoid discharge was widespread in New Zealand even though patients had good access to prosthetic eye services.
View the article here: Biosocial profile of New Zealand prosthetic eye wearers.
A search of the literature and of ocular prosthetists’ websites was undertaken to investigate what was known about the causes of discharge and to gain an understanding of the range of treatments for mucoid discharge associated with prosthetic eye wear. This search produced a comprehensive list of known specific causes of mucoid discharge but there remained a large and under-investigated group of patients with non-specific discharge for which many contradictory and inconsistent causes and treatments had been postulated. A survey of members of the American Society of Ocularists in 2007 carried out by K. L. Osborn and D. Hettler also found that a standardised set of treatment protocols for managing discharge was lacking.
View the article here: A survey of prosthetic eye wearers to investigate mucoid discharge.

Photographic scales developed by Dr Pine to measure deposits and conjunctival redness.

Laboratory equipment used to measure protein deposition on prosthetic eye material.
Further analysis of the responses from the New Zealand survey provided evidence of an association between the frequency of prosthetic eye cleaning and severity of discharge. Unfortunately, the direction of cause and effect could not be established – either frequent cleaning was causing the discharge or the discharge itself was the reason patients cleaned more frequently. To resolve this issue, further research into the socket’s response to prosthetic eye wear was planned. This research involved an examination of surface deposition on prosthetic eyes (which 47% of ocular prosthetists’ websites claimed was a main cause of mucoid discharge) and examination of the conjunctiva of the anophthalmic socket.
View the article here: Deposit build-up on prosthetic eyes and the implications for conjunctival inflammation and mucoid discharge.
However, surface deposits could not be investigated unless a technique was found to enable them to be seen, and neither deposits nor the conjunctiva could be examined unless measuring tools were developed for this purpose. A staining technique to make surface deposits more visible was found, and for the first time it was possible to investigate changes in the amount and extent of deposition on prosthetic eyes. It was then necessary to develop and test equal-interval photographic grading scales to measure these changes. At the same time, equal-interval photographic grading scales were also developed to measure the severity of conjunctival inflammation in anophthalmic sockets.
View the article here: The development of measuring tools for prosthetic eye research.

The wettabilty of a prosthetic eye surface is being measured with a goniometer.
The staining technique and the tools to measure surface deposition on prosthetic eyes and the severity of conjunctival inflammation were used successfully to provide a quantitative assessment of prosthesis cleaning effectiveness and to identify associations between deposits and discharge and deposits and conjunctival inflammation. Again, the direction of cause and effect of these associations could not be established at that stage. Evidence was found, however, that suggested that surface deposits themselves did not inflame the conjunctiva or cause discharge in anophthalmic sockets where the prosthesis was cleaned infrequently.
View the article: A survey of prosthetic eye wearers to investigate mucoid discharge.
The next set of experiments was designed to understand more about the characteristics of deposition and to find if a causal link could be established for the association between deposits, inflammation and discharge. The experiments involved both in-vitro and in-vivo tests of surface wettability and deposition rates on different prosthetic eye surface finishes. It was found from these experiments that rates of deposition were influenced by surface finish and that the presence of deposits caused a significant improvement in surface wettability. It seemed likely that the improved surface wettability would allow prosthetic eyes to be lubricated more effectively by the socket fluids, thereby reducing mechanical irritation of the conjunctiva. The evidence was building to suggest that the presence of at least some deposits was not only not harmful, but actually beneficial, causing reduced conjunctival inflammation and discharge in anophthalmic sockets with prosthetic eyes.
View the articles here:
The response of the anophthalmic socket to prosthetic eye wear.
Deposit buildup on prosthetic eye material (in vitro) and its effect on surface wettability.
This concept was further explored in the next study. It described the build-up of deposits over time and investigated the two distinctly different areas of deposition revealed by the deposit staining process: the inter-palpebral zone where stained deposits are mostly absent and the areas in continuous contact with the conjunctiva where deposits mostly settle. The deposits in the inter-palpebral zone appeared to behave like deposits on contact lenses where they may dry out and irritate the palpebral conjunctiva, whereas the presence of deposits elsewhere on the prosthesis appeared to be beneficial.
The combined results of all the investigations culminated in a hypothesis for a three-phase model of the anophthalmic socket’s response to prosthetic eye wear and a protocol for the management of non-specific mucoid discharge.
View the article here: A proposed model of the response of the anophthalmic socket to prosthetic eye wear and its application to the management of mucoid discharge.